Galtrey, CM;
Modarres, H;
Jaunmuktane, Z;
Brandner, S;
Rossor, AM;
Lockwood, DN;
Reilly, MM;
... Schon, F; + view all
(2017)
Leprosy in a patient infected with HIV.
Practical Neurology
, 17
(2)
pp. 135-139.
10.1136/practneurol-2016-001519.

Preview |
Text
Reilly_Galtrey et al 01.11.16 Leprosy and HIV.pdf Download (266kB) | Preview |
![[thumbnail of Figure 1high res.jpg]](https://discovery-pp.ucl.ac.uk/1533138/8.hassmallThumbnailVersion/Figure%201high%20res.jpg)  Preview |
Image
Figure 1high res.jpg - Accepted Version Download (715kB) | Preview |
![[thumbnail of Figure 2 PATH revised.jpg]](https://discovery-pp.ucl.ac.uk/1533138/15.hassmallThumbnailVersion/Figure%202%20PATH%20revised.jpg) 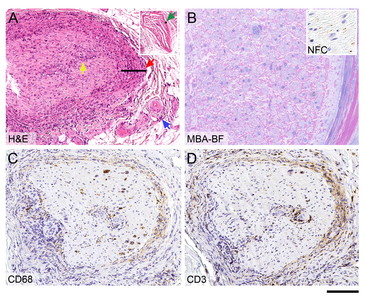 Preview |
Image
Figure 2 PATH revised.jpg - Accepted Version Download (1MB) | Preview |
Abstract
A 60-year-old Nigerian man, who had lived in Europe for 30 years but had returned home frequently, presented with right frontalis muscle weakness and right ulnar nerve palsy, without skin lesions. Neurophysiology showed a generalised neuropathy with demyelinating features. Blood tests were positive for HIV, with a normal CD4 count. There was nerve thickening both clinically and on MRI. Nerve biopsy showed chronic endoneuritis and perineuritis (indicating leprosy) without visible mycobacteria. His neuropathy continued to deteriorate (lepra reaction) before starting treatment with WHO multidrug therapy, highly active antiretroviral therapy and corticosteroids. There are 10 new cases of leprosy diagnosed annually in the UK. Coinfection with HIV is rare but paradoxically does not usually adversely affect the outcome of leprosy or change treatment. However, permanent nerve damage in leprosy is common despite optimal therapy. Leprosy should be considered in patients from endemic areas who present with mononeuritis multiplex.
Archive Staff Only
 |
View Item |


